Low Dose Radiation Therapy
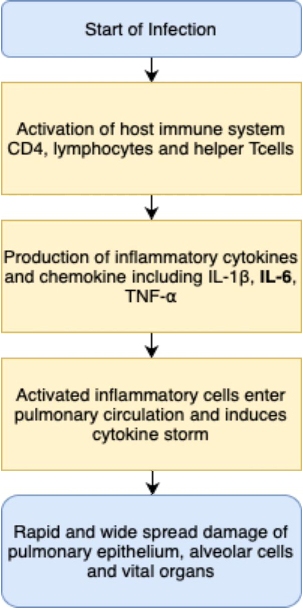
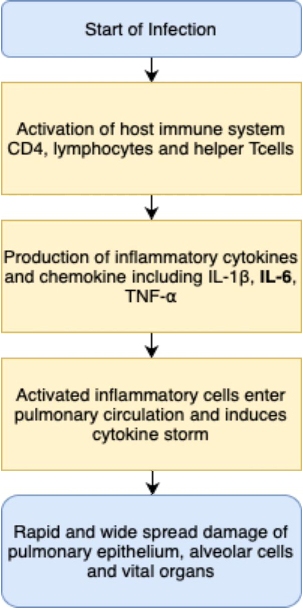
COVID19 pandemic has wreaked havoc on the healthcare system in every part of the world. The clinical effects of COVID19 range from asymptomatic infection, mild upper respiratory tract illness to severe pneumonia with respiratory failure, multi organ dysfunction and death. The unrestrained systemic inflammatory response in COVID19 triggers activation of inflammatory cells, this phenomena is commonly known as cytokine storm which inturn can induce Acute respiratory distress syndrome (ARDS) which is the leading cause of deaths. The COVID 19 pneumonia is different from other pneumonia in the way it progresses rapidly and in the exponential increase in inflammatory markers.
Thus It is of paramount importance to incorporate new treatment methods to augment the current treatment modalities. One such modality is the Low Dose Radiation Therapy (LDRT) which as per evidence of preliminary studies and trials conducted by several medical institutions is very promising.
Mechanism of LDRT[1-6]
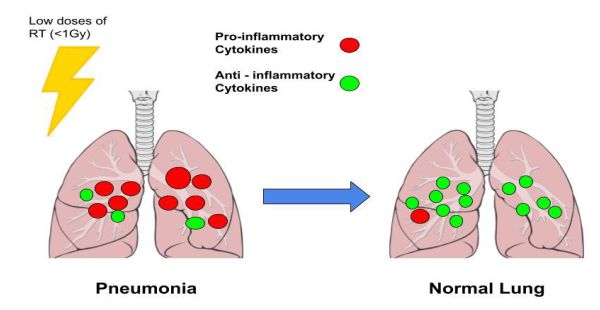
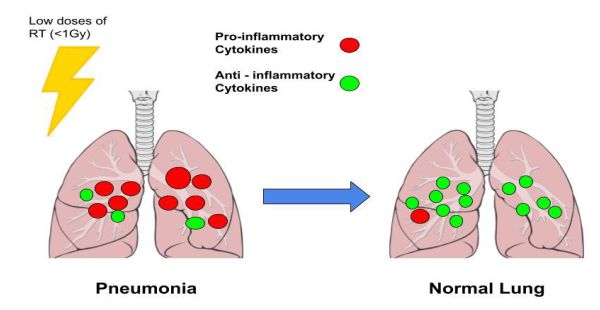
Radiation therapy is immunomodulatory, at doses lower than 1 Gy it exhibits anti-inflammatory effects and at higher doses above 1Gy it exhibits pro-inflammatory effects.
Low Dose Radiotherapy at 0.5 Gy is a non-toxic, cost effective, evidence based anti-inflammatory therapeutic tool that has the potential to improve the respiratory complications and avoid the complications of cytokine storm.
Low dose radiation therapy and has an anti-inflammatory effect at low doses which is mediated by the suppression of pro-inflammatory cytokines such as IL6 (IL6 levels are elevated in severe cases of COVID 19) and induction of anti-inflammatory cytokines such as IL10.
LD-RT treatment (30–100 cGy) to the lungs of SARS-COV 2 patients could taper off the pneumonia associated inflammation by creating an anti-inflammatory environment and also lessen the probability of death.
Workflow of LDRT
The workflow of Radiotherapy is quite simple it includes :
1. Transport of patient to the radiotherapy unit
2. Treatment planning and scheduling
3. Treatment position immobilization
4. Treatment delivery and monitoring during treatment – the patient’s thoracic region is irradiated with low doses of radiation (less than 1Gy) by a radiotherapy device such as a linear accelerator (Linac).
5. Transporting back
This entire procedure may take up to 10-15 minutes.
How is Outcome Measured
1. Symptomatic improvement or deterioration by comparing NEWS score with post LDRT score on days 3, 4, 7 and 14
2. Length of hospital stay post LDRT
3. Number of ICU admissions/deaths
Advantages of LDRT
1. Single fraction treatment : short and quick
2. It’s a non consumable treatment : unlike vaccine or drug
3. It has no impact on viral mutation : No selective pressure is applied on the virus
4. Existing Radiotherapy infrastructure can be utilised
5. Preventing ICU admissions : Need of the hour and huge benefit for India
a. No ICU setup required
b. No ventilator required
c. Less need of ICU staff (minimise deaths in healthcare workers)
Challenges
1. Ethical Approval : Treating infection by radiation
2. Fear of infection among radiation team : non covid team (medical physicists, RT technologists ) being potentially exposed to COVID 19
3. Logistical Issues – Sanitising the RT machines and transporting the COVID positive patients to the radiotherapy unit.
4. Interference with treatment of cancer patients as the same radiotherapy machines will be used for LDRT purposes as well.
5. Cancer Risk : Radiation therapy being used for benign conditions does raise concerns about the risk of radiation induced carcinogenesis.
6. Determining the right time for intervention by this method – if this therapy is given at a very early stage of the infection, it might compromise the body’s ability to fight of infection on it’s own and might be futile if given very late.
Recent trials conducted by various medical institutions suggests that :
1. LDRT is safe and well tolerated by patients
2. No acute toxicities were observed
3. O2 demand reduces ealy on in majority of patients
4. Very good early radiographic response
Conclusion
LDRT can prevent cytokine storm (which leads to ARDS and multi-organ failure) thereby preventing further deterioration of the patient and reducing the mortality when given at the right time. It also has the potential to reduce post COVID lung sequelae. Furthermore, it can reduce burden on healthcare systems by reducing the dependence on oxygen, need of mechanical ventilation and intubation. With more trials, studies and data validating this approach, it can be considered as a potential standardised treatment for severe cases.
References
1. Calabrese E, Dhawan G. How radiotherapy was historically used to treat pneumonia: Could it be useful today? . Yale J Biol Med. 2013.
2. DN Sharma, Randeep Guleria. Low Dose Radiation Therapy for COVID-19 Pneumonia: A Pilot Study. 2020
3. Kirby, Charles, and Marc Mackenzie. Is low dose radiation therapy a potential treatment for COVID-19 pneumonia? 2020
4. Meziani, Lydia, and Charlotte Robert. “Low Doses of Radiation Increase the Immunosuppressive Profile of Lung Macrophages During Viral Infection and Pneumonia.” International Journal of Radiation Oncology*Biology*Physics, 2021.
5. F. Rodel, B. Frey, U. Gaipl, L. Keilholz, C. Fournier, K. Manda, H. Schollnberger, G. Hildebrandt and C. Rodel, “Modulation of Inflammatory Immune Reactions by Low-Dose Ionizing Radiation: Molecular Mechanisms and Clinical Application”, Current Medicinal Chemistry (2012) 19: 1741. https://doi.org/10.2174/092986712800099866
6. Sharma, DN, and Rishabh Kumar. “Low-dose radiotherapy for COVID 19: A radioimmunological perspective.
Kartikeya Sethi is currently working on understanding the effects of low dose ionising radiation on the human body for treating benign conditions, primarily the COVID19 infection in order to make the treatment by Low Dose Radiation Therapy a safe option.
He can be contacted by email at kartikaymsvv@gmail.com